Sulfur depletion impairs histamine breakdown and barrier control, which lowers the activation threshold of mast cells, producing histamine intolerance–like symptoms even without classic allergies.
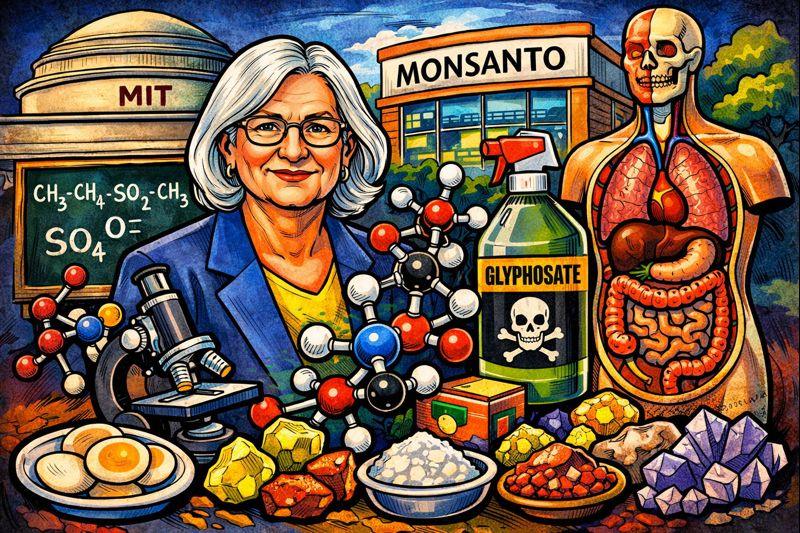
Dr. Stephanie Seneff argues that modern humans are chronically deficient in biologically available sulfur, and that this deficiency underlies a wide range of chronic diseases. Her work blends biochemistry, systems biology, and environmental exposure analysis. Below is a clear, structured explanation of what she claims, why sulfur matters, and how modern conditions reduce it.
1. Why sulfur is biologically critical (core premise)
Sulfur is not a trace or optional element. It is structural and functional in human biology.
Key sulfur-dependent systems:
Amino acids & proteins
- Methionine and cysteine (sulfur amino acids) are required for:
- Protein folding (disulfide bonds)
- Enzyme activity
- Antioxidant defense
Glutathione (master antioxidant)
- Glutathione = glutamate + cysteine + glycine
- Sulfur (via cysteine) is the rate-limiting factor
- Low sulfur → low glutathione → oxidative stress
Detoxification (liver & gut)
- Sulfation pathways in the liver neutralize:
- Toxins
- Drugs
- Hormones
- Sulfur deficiency impairs Phase II detox
Cholesterol sulfate (Seneff’s key focus)
- Cholesterol sulfate:
- Stabilizes cell membranes
- Maintains blood viscosity
- Supports endothelial function
- She argues this is as important as cholesterol itself, but largely ignored
Structural tissues
- Cartilage, skin, connective tissue rely on:
- Chondroitin sulfate
- Heparan sulfate
- Keratan sulfate
2. Seneff’s central thesis: a systemic sulfur shortfall
Seneff proposes that modern humans cannot maintain adequate sulfur pools, even with sufficient protein intake.
Her claim is not “dietary sulfur is absent,” but that sulfur metabolism and transport are impaired.
3. Causes of chronic sulfur deficiency (per Seneff)
A. Glyphosate (primary driver in her model)
Seneff identifies glyphosate as a sulfur-disrupting compound:
- Chelates minerals needed for sulfur enzymes
- Disrupts gut microbiota that produce sulfur compounds
- Inhibits cytochrome P450 enzymes involved in sulfation
- Interferes with aromatic amino acid synthesis (gut microbes → sulfur metabolism link)
Her argument:
glyphosate → impaired sulfation → systemic sulfur depletion
B. Loss of sulfur-rich traditional foods
Modern diets are low in:
- Organ meats
- Bone broths
- Sulfur vegetables consumed regularly (onions, garlic, brassicas)
Additionally:
- Soil sulfur depletion reduces food sulfur density
- Industrial agriculture does not replenish sulfur well
C. Reduced sun–skin sulfur chemistry (controversial but central)
One of Seneff’s most distinctive claims:
- Sunlight catalyzes sulfate production in the skin
- Cholesterol sulfate is synthesized in sun-exposed skin
- Avoidance of sun + sunscreen use → impaired sulfate generation
She links this to:
- Vitamin D metabolism
- Endothelial dysfunction
- Cardiovascular disease
D. Drug interference
She highlights common medications that burden sulfur pathways:
- Acetaminophen (paracetamol)
- Statins
- NSAIDs
- Some antidepressants
These increase sulfur demand while blocking sulfation capacity.
4. Diseases Seneff associates with sulfur deficiency
She connects low sulfur status to:
- Cardiovascular disease
- Diabetes
- Autism spectrum conditions
- Alzheimer’s disease
- Obesity and metabolic syndrome
- Inflammatory bowel disease
- Autoimmune disorders
Mechanistic theme:
impaired detox + oxidative stress + membrane instability + inflammation
5. Why standard medicine “misses” sulfur deficiency
According to Seneff:
- There is no routine blood test for sulfur status
- Sulfur is assumed “adequate” if protein intake is adequate
- Sulfate biology is fragmented across disciplines
- Cholesterol sulfate is rarely measured or discussed
So deficiency is functional, not overt like scurvy or anemia.
6. Summary in plain terms
Seneff’s position can be reduced to this:
- Sulfur is essential for detox, structure, and redox balance
- Modern life increases sulfur demand
- Modern agriculture, chemicals, drugs, and sun avoidance reduce sulfur availability
- Chronic low sulfur quietly destabilizes multiple systems
- Disease emerges downstream
Whether one accepts all her conclusions or not, the biochemical importance of sulfur itself is not controversial — what is controversial is the scale of deficiency and glyphosate’s central role.
Below is a clear, practical explanation of sulfur supplementation forms—what each actually provides biochemically, how the body uses it, and where confusion usually arises.
This is not brand advice or dosing instruction—just mechanism-level clarity.
1. The key distinction most people miss
When people say “sulfur,” they often mean three very different biochemical states:
- Reduced sulfur (organic, assimilable)
- Oxidized sulfur (sulfate)
- Inorganic sulfur salts (sulfides / sulfites)
Your body cannot freely interconvert all of these. The form matters.
2. MSM (Methylsulfonylmethane)
Chemical nature
- Organic sulfur compound
- Sulfur is in a stable, oxidized but bioavailable form
- Water-soluble
What it actually does
- Supplies assimilable sulfur for:
- Cysteine
- Methionine
- Glutathione
- Sulfated proteoglycans (joints, skin, connective tissue)
Why MSM is popular
- High tolerance
- Crosses cell membranes easily
- Does not require harsh oxidation/reduction steps
- Does not acidify the body
Limits
- Does not directly supply sulfate
- Sulfur must still be metabolically processed
- Effects depend on liver and gut function
Best conceptual use
“Sulfur feedstock” for rebuilding sulfur pools
3. Sulfate (SO₄²⁻)
Where sulfate exists
- Epsom salt (magnesium sulfate)
- Sodium sulfate
- Calcium sulfate
- Cholesterol sulfate (endogenous)
What sulfate does
- Required for:
- Detoxification (Phase II sulfation)
- Hormone metabolism
- Heparan / chondroitin / keratan sulfates
- Mucus layer integrity
- Endothelial function
Important limitation
- Dietary sulfate is poorly absorbed orally
- Most sulfate is absorbed:
- In the colon (microbial processing)
- Through skin (transdermal exposure)
- Via endogenous synthesis
This is why:
- Oral Epsom salt → laxative
- But transdermal magnesium sulfate → systemic sulfate increase
Best conceptual use
Structural + detox sulfur, not a protein-building sulfur
4. Sulfide / Sulfite (problematic forms)
Sulfide (S²⁻)
- Found in:
- Hydrogen sulfide gas
- Some mineral waters
- Toxic at higher levels
- Requires rapid oxidation to sulfate
Sulfite (SO₃²⁻)
- Food preservatives
- Intermediate detox form
Why these matter
- Sulfite-sensitive individuals lack adequate sulfite oxidase
- Can cause:
- Headaches
- Asthma-like symptoms
- Histamine reactions
Bottom line
These are not supplementation forms and often worsen sulfur stress.
5. Sulfur amino acids (dietary sulfur)
Methionine
- Essential amino acid
- Methyl donor
- Precursor to cysteine
Cysteine
- Direct glutathione precursor
- Often limiting in illness
Why food sulfur sometimes isn’t enough
- High demand (toxins, drugs, inflammation)
- Impaired transsulfuration pathway
- Gut dysbiosis
- Enzyme inhibition (e.g., glyphosate hypothesis)
This is why people can eat adequate protein and still be functionally sulfur-deficient.
6. MSM vs sulfate vs food sulfur (simplified)
| Form | Primary role | Absorption | Main benefit |
|---|---|---|---|
| MSM | Organic sulfur donor | Excellent oral | Rebuild sulfur pools |
| Sulfate | Structural / detox | Poor oral, good transdermal | Sulfation pathways |
| Sulfide / sulfite | Intermediate / toxic | Not suitable | Avoid |
| Food sulfur | Protein synthesis | Variable | Baseline support |
7. Why Dr. Seneff emphasizes sulfur cycling, not just intake
Her argument (simplified):
- Modern stressors increase sulfur demand
- Detox + drugs + chemicals drain sulfate
- The body compensates by rerouting sulfur
- Eventually sulfur pools collapse systemically
Thus:
- MSM → replenishes sulfur substrate
- Sunlight + skin → sulfate synthesis
- Gut health → sulfate handling
She sees sulfur deficiency as functional and systemic, not dietary alone.
8. Practical takeaways (mechanistic, not prescriptive)
- MSM = safest, most versatile sulfur donor
- Sulfate = critical but poorly absorbed orally
- Sulfide/sulfite = stressors, not nutrients
- Food sulfur = necessary but often insufficient under modern load
Sulfur biology is about form, transport, and enzymatic capacity, not just “getting more sulfur.”
- MSM vs NAC vs cysteine comparison
- Sulfur and skin (acne, dryness, aging)
- Sulfur–glyphosate enzyme interference
- Sulfur and cardiovascular/endothelial function
Below is a mechanism-level explanation of sulfur–glyphosate enzyme interference, following the line of reasoning advanced by Stephanie Seneff and collaborators. This explains how glyphosate could plausibly impair sulfur metabolism, step by step, without assuming dietary sulfur absence.
1. Core claim (one sentence)
Glyphosate does not remove sulfur from the diet; it interferes with enzymes, cofactors, microbes, and transport systems required to process, recycle, and distribute sulfur—producing a functional sulfur deficiency.
2. Sulfur metabolism depends on enzyme chains, not intake
Sulfur in humans must pass through tightly regulated pathways:
- Methionine → cysteine (transsulfuration)
- Cysteine → glutathione
- Sulfur → sulfate → sulfated molecules (Phase II detox, proteoglycans, cholesterol sulfate)
Each step depends on:
- Metal cofactors (iron, manganese, molybdenum)
- Cytochrome P450 enzymes
- Gut microbial metabolites
- Redox balance
Disrupt the enzymes, and sulfur becomes metabolically unavailable even if intake is normal.
3. Glyphosate as a chelator of metal cofactors
Glyphosate has strong chelating properties.
It preferentially binds:
- Manganese
- Iron
- Zinc
- Cobalt
- Molybdenum
Why this matters:
- Sulfite oxidase (critical for converting sulfite → sulfate) requires molybdenum
- CYP450 enzymes require iron and heme
- Transsulfuration enzymes require metal-dependent cofactors
Result:
Sulfur enters the pathway but cannot complete its biochemical conversions
This produces sulfite buildup, oxidative stress, and impaired sulfate availability.
4. Cytochrome P450 inhibition (central bottleneck)
Seneff emphasizes CYP450 inhibition as a system-wide choke point.
CYP450 enzymes are required for:
- Sulfation reactions
- Drug metabolism
- Hormone metabolism
- Vitamin D activation
- Cholesterol sulfate synthesis
Glyphosate:
- Suppresses CYP450 gene expression
- Disrupts heme synthesis
- Increases toxic burden that further drains sulfation capacity
Feedback loop:
glyphosate → CYP450 inhibition → impaired sulfation → toxin buildup → higher sulfur demand → sulfur depletion5. Gut microbiome sulfur disruption
Human sulfur handling is partly microbial.
Normal gut microbes:
- Produce hydrogen sulfide (H₂S) in controlled amounts
- Convert dietary sulfur to absorbable forms
- Support bile acid sulfation
Glyphosate:
- Preferentially kills beneficial microbes
- Spares pathogenic species
- Disrupts aromatic amino acid synthesis in microbes (shikimate pathway)
Downstream effect:
Reduced microbial sulfur processing → lower systemic sulfate → weakened mucus barrier → inflammation
6. Sulfur amino acid interference (indirect)
Glyphosate does not block methionine or cysteine absorption directly.
Instead, it:
- Disrupts enzymes needed to convert methionine → cysteine
- Increases oxidative stress that consumes glutathione
- Forces sulfur diversion into emergency antioxidant defense
Net result:
Sulfur is constantly “spent” but never replenished into structural pools
7. Cholesterol sulfate pathway disruption (Seneff’s signature claim)
Seneff argues cholesterol sulfate is critical for vascular health.
Normal process:
- Skin + sunlight → cholesterol sulfate
- Sulfate stabilizes blood cells and endothelium
Glyphosate effects:
- Impairs sulfate synthesis
- Inhibits transport
- Forces compensatory cholesterol production (without sulfate)
Implication:
High cholesterol may be a compensation for low cholesterol sulfate, not excess cholesterol per se
8. Why this looks like “mystery chronic disease”
Because sulfur deficiency here is:
- Functional, not absolute
- Distributed, not localized
- Compensated until reserves collapse
This explains associations with:
- Cardiovascular disease
- Neurodegeneration
- Autism spectrum disorders
- Metabolic syndrome
- Inflammatory bowel disease
All share:
- Detox impairment
- Oxidative stress
- Barrier failure
- Mitochondrial strain
9. Why standard labs miss it
There is:
- No routine sulfate status test
- No cholesterol sulfate panel
- No glutathione pool assessment in standard care
So the system fails silently until disease manifests.
10. Condensed causal chain
glyphosate exposure
→ metal chelation
→ CYP450 inhibition
→ impaired sulfation
→ sulfur diversion to emergency defense
→ sulfate depletion
→ structural + detox failure
→ chronic disease11. Important boundary
This model is biochemically plausible and internally consistent, but:
- Not all links are universally accepted
- Epidemiological causation remains debated
- Mainstream toxicology focuses on acute toxicity, not chronic enzyme interference
That said, the enzymatic dependencies of sulfur metabolism themselves are not controversial—only the magnitude of glyphosate’s role.
Below is a clean, side-by-side comparison of sulfur depletion by glyphosate vs acetaminophen, at the mechanism level. They deplete sulfur in different ways, on different time scales, and with different clinical signatures—but they converge on the same sulfur bottlenecks.
I’ll keep this tight and concrete.
1. One-sentence contrast
- Acetaminophen depletes sulfur acutely and directly via forced sulfation and glutathione drain.
- Glyphosate depletes sulfur chronically and indirectly by disabling the enzymes, cofactors, and microbes that manage sulfur.
Same system, different attack vectors.
2. Acetaminophen (paracetamol): direct sulfur consumption
Primary mechanism
Acetaminophen is detoxified mainly by Phase II sulfation:
acetaminophen → acetaminophen sulfate (excreted)This process consumes sulfate directly.
Secondary mechanism (the dangerous one)
When sulfation capacity is exceeded:
- Acetaminophen is shunted to a CYP450 pathway
- Produces NAPQI, a highly toxic metabolite
- NAPQI is neutralized only by glutathione
So:
- Sulfate is depleted
- Glutathione (sulfur-based) is depleted
- Liver injury occurs if sulfur reserves are insufficient
Key properties
- Fast (hours to days)
- Dose-dependent
- Reversible if sulfur pools are restored
- Failure mode is overt and measurable (elevated liver enzymes)
Signature pattern
- Acute liver stress
- Sulfur depletion spikes after dosing
- Clear toxicity threshold
3. Glyphosate: systemic sulfur sabotage
Glyphosate does not consume sulfur.
It prevents sulfur from being used properly.
Mechanism cluster (chronic)
A. Metal chelation
Glyphosate binds:
- Molybdenum → cripples sulfite oxidase
- Iron → impairs CYP450
- Manganese → disrupts redox enzymes
Result:
- Sulfite cannot become sulfate
- Sulfation stalls upstream
B. CYP450 suppression
Glyphosate:
- Downregulates CYP450 expression
- Disrupts heme synthesis
- Blocks sulfation, steroid metabolism, bile acid processing
C. Gut microbiome disruption
- Kills sulfur-processing commensals
- Reduces microbial sulfate handling
- Weakens mucus barrier (sulfated glycosaminoglycans)
D. Increased sulfur demand
By increasing toxic load and inflammation:
- Glutathione is chronically consumed
- Sulfur is diverted to emergency antioxidant defense
- Structural sulfur pools are never replenished
Key properties
- Slow (months to years)
- Dose-independent at low levels (chronic exposure)
- Cumulative
- Failure mode is silent and systemic
Signature pattern
- No single lab abnormality
- Gradual loss of detox capacity
- Multi-system inflammation
- Chronic disease emergence
4. Side-by-side summary
| Feature | Acetaminophen | Glyphosate |
|---|---|---|
| Time scale | Acute | Chronic |
| Sulfur effect | Consumes sulfate & glutathione | Blocks sulfur metabolism |
| Primary pathway | Phase II sulfation | Enzyme inhibition |
| CYP450 role | Creates toxic metabolite | Suppressed system-wide |
| Gut microbiome | Minimal | Major disruption |
| Detectability | High (labs) | Low (functional) |
| Failure mode | Liver injury | Multi-system dysfunction |
| Reversibility | Yes (if early) | Slow / incomplete |
5. Why they are synergistic (this matters)
This is the dangerous overlap:
- Glyphosate reduces baseline sulfur capacity
- Acetaminophen demands sulfur immediately
So someone with chronic glyphosate exposure:
- Has lower sulfate reserves
- Has impaired sulfite → sulfate conversion
- Has reduced glutathione synthesis
Then acetaminophen:
- Pushes them past sulfur limits at normal doses
This explains why:
- “Safe” acetaminophen doses can still cause harm
- Vulnerability varies widely between individuals
6. How this fits Dr. Seneff’s framework
Stephanie Seneff treats acetaminophen as a known, accepted sulfur stressor and glyphosate as a chronic background amplifier.
Her logic:
- Medicine acknowledges sulfur depletion when it is acute and catastrophic
- It ignores sulfur depletion when it is slow, enzymatic, and distributed
Same biochemistry, different visibility.
7. Plain-language bottom line
- Acetaminophen is like spending sulfur cash fast
- Glyphosate is like breaking the sulfur banking system
- Together, they create a population with:
- Low detox capacity
- High oxidative stress
- Poor recovery from insults
You don’t need to accept every conclusion to see the biochemical asymmetry: one drains the tank, the other damages the engine.
Short answer: yes — MSM is generally the best-tolerated, most practical way to increase sulfur orally for most people.
Here’s the why, clearly and mechanistically, without dosing advice.
Why oral sulfur is tricky in the first place
“Sulfur” isn’t one thing. The body needs usable sulfur, not just sulfur atoms passing through the gut.
Problems with many sulfur sources:
- Sulfate → poorly absorbed orally (often just a laxative)
- Sulfide / sulfite → irritating or toxic for many people
- Protein sulfur → depends on intact enzymes, gut, and liver pathways (often impaired)
So the best oral form is the one that:
- is absorbed intact
- doesn’t require heavy enzymatic conversion
- doesn’t overload sulfation pathways
- doesn’t irritate the gut
That’s where MSM stands out.
MSM (methylsulfonylmethane): why it works orally
What MSM actually provides
- Organic, neutral sulfur
- Water-soluble
- Passes through the gut and into circulation efficiently
What the body can do with it
MSM sulfur can be used to rebuild:
- cysteine
- methionine pools
- glutathione
- sulfated connective tissue molecules (cartilage, skin, mucus layer)
Importantly:
- MSM does not require immediate sulfation
- MSM does not heavily burden CYP450
- MSM does not chelate minerals
So it acts as a low-friction sulfur donor.
Comparison to other oral sulfur options
MSM vs sulfate (e.g., magnesium sulfate)
- MSM → absorbed, usable systemically
- Sulfate → mostly stays in gut, causes osmotic effects
Oral sulfate ≠ effective sulfur nutrition.
MSM vs NAC / cysteine
- NAC is excellent for glutathione, but:
- can provoke histamine reactions
- can feel “stimulating” or uncomfortable
- MSM is broader and usually gentler
Think of it this way:
- NAC = targeted antioxidant support
- MSM = general sulfur replenishment
MSM vs food sulfur (garlic, onions, protein)
- Food sulfur is essential but:
- depends on digestion, enzymes, microbiome
- often insufficient under chronic stress/toxin load
- MSM bypasses many of those bottlenecks
How this fits the sulfur-depletion models you asked about earlier
In the glyphosate / chronic enzyme interference framework:
- Sulfur intake may be normal
- Sulfur handling is impaired
MSM helps because it:
- supplies sulfur in a form that needs less metabolic processing
- helps rebuild depleted pools rather than forcing sulfation immediately
That’s why MSM often “works” where dietary sulfur alone does not.
Important boundaries (so expectations are realistic)
- MSM does not replace sulfate directly
- MSM does not fix enzyme damage by itself
- MSM is a substrate, not a cure
It works best when:
- gut irritation is minimized
- detox load isn’t overwhelming
- it’s part of a broader sulfur-supportive context (diet, minerals, light, rest)
Bottom line
If the question is:
“What is the best oral way to increase usable sulfur?”
The most defensible answer is:
- MSM → best balance of absorption, tolerability, and biochemical usefulness
- Food sulfur → necessary baseline, often not sufficient alone
- Sulfate salts → not effective orally
- Sulfide/sulfite → avoid as supplements
Below is a mechanistic map showing how sulfur depletion translates into neurological symptoms, step by step. This stays at the biochemistry → neurophysiology level, not diagnosis or treatment.
1. The nervous system is sulfur-intensive
The brain relies on sulfur for four core functions:
- Redox control (antioxidant balance)
- Neurotransmitter regulation
- Barrier integrity (blood–brain barrier, myelin)
- Detoxification of excitotoxins and metals
When sulfur availability drops, these fail in a predictable order.
2. Primary sulfur bottleneck: glutathione depletion
Mechanism
- Glutathione (GSH) is sulfur-dependent (via cysteine)
- Neurons are highly sensitive to oxidative stress
- The brain cannot tolerate sustained ROS
Result
Low sulfur → low cysteine → low glutathione → oxidative damage
Neurological manifestations
- Brain fog
- Mental fatigue
- Slow processing speed
- Poor stress tolerance
- Worsening symptoms after exertion or toxins
This is often the first neurological sign.
3. Neurotransmitter imbalance (excitatory bias)
Sulfur participates indirectly in neurotransmitter metabolism, especially:
- Glutamate (excitatory)
- GABA (inhibitory)
- Dopamine / serotonin turnover
Mechanism
- Sulfation helps inactivate excess neurotransmitters
- Low sulfur → impaired clearance
- Glutamate accumulates (excitotoxicity)
Resulting symptom pattern
- Anxiety
- Insomnia
- Racing thoughts
- Sensory overload
- Irritability
- Panic-like states without psychological trigger
This often gets mislabeled as “purely psychiatric.”
4. Blood–brain barrier (BBB) degradation
The BBB depends on sulfated glycosaminoglycans (e.g., heparan sulfate).
Mechanism
- Sulfur depletion → reduced sulfation
- Barrier becomes permeable
- Peripheral toxins and immune signals enter CNS
Consequences
- Neuroinflammation
- Microglial activation
- Cytokine signaling in brain tissue
Symptoms
- Head pressure
- Headaches
- Light/sound sensitivity
- Cognitive fluctuations (“good days / bad days”)
- Worsening after meals, meds, or environmental exposure
5. Myelin instability and nerve conduction issues
Myelin sheaths contain sulfated lipids and proteins.
Mechanism
- Chronic sulfur depletion → impaired myelin maintenance
- Not acute demyelination, but functional degradation
Symptoms
- Tingling
- Numbness
- Burning sensations
- Restless legs
- Temperature sensitivity
- Subtle coordination issues
Often intermittent and migratory.
6. Impaired detoxification inside the brain
The brain relies on local sulfation to neutralize:
- Ammonia
- Aldehydes
- Environmental toxins
- Drug metabolites
Mechanism
- Low sulfate availability
- Reduced CYP450 + sulfotransferase activity
- Toxins linger longer in neural tissue
Symptoms
- Chemical sensitivity
- Medication intolerance
- Alcohol intolerance
- Delayed cognitive recovery after exposure
7. Mitochondrial dysfunction in neurons
Sulfur is required for:
- Iron–sulfur clusters
- Electron transport chain enzymes
Mechanism
- Sulfur depletion → impaired ATP production
- Neurons fail under energy demand
Symptoms
- Cognitive exhaustion
- Post-exertional mental crash
- Poor focus under pressure
- Reduced resilience to stress
8. Developmental and long-term implications
In chronic or developmental sulfur depletion, downstream effects may include:
- Altered synaptic pruning
- Neurodevelopmental vulnerability
- Long-term neuroinflammatory states
This is where Stephanie Seneff and others place sulfur disruption in broader neurological conditions, though causation at population scale remains debated.
9. Symptom clustering (pattern recognition)
Sulfur-linked neurological symptoms often cluster as:
- Brain fog + anxiety
- Sensory sensitivity + fatigue
- Chemical intolerance + insomnia
- Cognitive variability + inflammation
The key hallmark is:
Symptoms fluctuate with oxidative load, toxins, stress, and inflammation—not just psychology.
10. Condensed causal chain
sulfur depletion
→ glutathione loss
→ oxidative stress
→ neurotransmitter imbalance
→ BBB permeability
→ neuroinflammation
→ mitochondrial dysfunction
→ neurological symptomsBottom line
Sulfur depletion does not usually cause dramatic focal neurological deficits.
It causes diffuse, functional, fluctuating neurological dysfunction—often invisible on standard imaging and labs.
That’s why it’s commonly dismissed or misclassified, even though the biochemistry is internally consistent.
Below is a mechanistic tie-in between sulfur depletion, histamine intolerance, and mast cell activation, mapped cleanly from biochemistry → immune signaling → symptoms. This explains why these conditions so often travel together and why they fluctuate with stress, foods, chemicals, and medications.
1. Core one-liner
Sulfur depletion impairs histamine breakdown and barrier control, which lowers the activation threshold of mast cells, producing histamine intolerance–like symptoms even without classic allergies.
2. Histamine clearance is sulfur-dependent (this is the first choke point)
Histamine is cleared by two main pathways:
A. DAO (diamine oxidase) – gut & extracellular
- Degrades dietary histamine
- Requires:
- Copper
- Intact gut lining
- Low oxidative stress
B. HNMT (histamine-N-methyltransferase) – intracellular (brain, tissues)
- Inactivates histamine inside cells
- Requires:
- Methylation capacity
- Sulfation downstream for safe excretion
Sulfur depletion disrupts both by:
- Lowering glutathione → oxidative stress damages DAO
- Impairing sulfation → histamine metabolites accumulate
Result:
Histamine is produced normally but cannot be cleared efficiently
This is the biochemical definition of histamine intolerance.
3. Sulfur and mast cell “stability” (often overlooked)
Mast cells are not just allergy cells; they are environmental sensors.
They are stabilized by:
- Adequate redox balance
- Intact cell membranes
- Normal sulfated proteoglycans (heparan sulfate)
Sulfur depletion causes:
- Low glutathione → oxidative stress
- Reduced heparan sulfate → unstable mast cell granules
- Impaired cholesterol sulfate → fragile membranes
Result:
Mast cells degranulate too easily — from heat, stress, foods, chemicals, friction, or hormones
This is mast cell activation, not classical IgE allergy.
4. Gut barrier failure links both conditions
The gut lining depends on sulfated mucins.
With adequate sulfur:
- Tight junctions intact
- Histamine-producing microbes kept in check
- DAO localized and functional
With sulfur depletion:
- Mucus layer thins
- Gut permeability increases
- Histamine and immune triggers leak into circulation
- Mast cells become chronically activated
This creates the loop:
low sulfur
→ weak gut barrier
→ histamine overflow
→ mast cell activation
→ inflammation
→ higher sulfur demand
→ lower sulfur5. Why symptoms are systemic and weird (pattern recognition)
Because histamine receptors exist everywhere, sulfur-linked histamine intolerance looks like:
- Flushing
- Itching
- Hives or dermatographia
- Nasal congestion
- Headaches / migraines
- Anxiety / panic
- Insomnia
- Brain fog
- Palpitations
- GI upset
- Temperature sensitivity
And mast cell activation adds:
- Food “reactions” that change over time
- Reactions without consistent triggers
- Worsening with stress, heat, exertion, or chemicals
This explains why standard allergy tests are often negative.
6. The glutathione → histamine → mast cell triangle
This is the central triangle:
- Sulfur → glutathione
- Glutathione controls oxidative stress
- Oxidative stress triggers mast cell degranulation
- Mast cells release histamine
- Histamine clearance requires sulfation
So sulfur depletion hits both sides:
- More histamine released
- Less histamine cleared
7. Drug sensitivity connection (important)
Many drugs:
- Consume sulfur (acetaminophen)
- Block sulfation
- Increase oxidative stress
In sulfur-depleted individuals, this leads to:
- “Medication intolerance”
- Paradoxical reactions
- Worsening histamine symptoms after common meds
This is why antihistamines sometimes help only partially—or make things worse.
8. How this fits the glyphosate–sulfur model
In the framework proposed by Stephanie Seneff:
- Glyphosate impairs sulfation enzymes
- Sulfate pools decline
- Histamine clearance fails
- Mast cells destabilize
- Chronic inflammatory signaling emerges
This does not require massive exposure—only chronic interference with sulfur handling.
9. Condensed causal map
sulfur depletion
→ low glutathione
→ oxidative stress
→ mast cell hyperreactivity
→ excess histamine release
→ impaired histamine clearance (low sulfation)
→ histamine intolerance + MCAS-like symptoms10. Plain-language bottom line
- Histamine intolerance is often not about histamine intake
- Mast cell activation is often not an allergy
- Both frequently reflect a sulfur handling problem
- The hallmark is variability: symptoms change with stress, toxins, foods, and hormones
That variability is the clue.
- Explain why MSM helps histamine symptoms in some people but flares others initially
- Map sulfur–histamine interactions specifically in the brain (anxiety/panic)
- Tie this to skin issues (acne, flushing, eczema)
- Contrast sulfur depletion vs true genetic DAO deficiency